Anatomy and Physiology: Reabsorption
Reabsorption
It's a bit ironic that once the material has been filtered out, so much of it is reabsorbed! Some of this makes sense when you look at the amounts. Remember that the GFR is 125 ml/minute; that adds up to 180 liters of filtrate a day. If we didn't reabsorb some of that material we would run out rather fast! Since we average about 5 liters of blood, and 55 percent of that is plasma, we would be out of fluid in 22 minutes! It turns out that we reabsorb between 178 to 179 liters a day. That leaves 1 to 2 liters to be urinated away every day. Think of that the next time you open a 2-liter soda bottle; for some reason the word humbling comes to mind!
Much of this movement of material starts right away in that twisted tube right off the glomerulus called the proximal convoluted tubule or PCT for short (see Figure 15.5). The inside of this tubule, like the cells on the outside of the villi of the small intestine (see The Digestive System), has a brush border of microvilli, which of course increases surface area for the reabsorption; the major difference here is the cuboidal shape of the cells, unlike the columnar cell of the villi. I am talking here about reabsorption into the blood, specifically into what are called peritubular (around the tubes) capillaries.
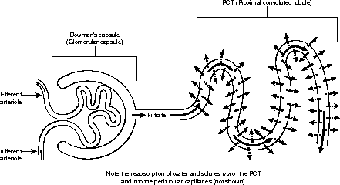
Figure 15.5Reabsorption in the PCT and descending loop of Henle. (©Michael J. Vieira Lazaroff)
You might remember that the movement of materials in and out of vessels occurs via both diffusion (which, as passive transport, requires no energy) and active transport (which, going against the concentration gradient, requires energy). For diffusion to occur there needs to be a difference in the concentration of material (solute or solvent) on both sides of the membranes. In addition, cells cannot perform active transport to reabsorb water, and so the only way to get the water back into the capillaries is to create osmotic pressure by greatly increasing the concentration of the blood (that is, making it hypertonic;). The easiest way to do this is to have a countercurrent mechanism.
A countercurrent mechanism means that the flow of the filtrate through the tubes passes in the opposite direction from the flow of the blood, despite both starting at the glomerulus in the Bowman's capsule: The filtrate goes directly from the glomerulus to the PCT and loop of Henle, and then to the DCT, whereas the capillaries go from the glomerulus, skip over to the DCT, and then move backward to the loop of Henle and the PCT.
In this way, increasing the concentration of Na+, Cl-, K+, and HCO3- in the capillaries (through reabsorption and secretion from the DCT and the ascending limb of the loop of Henle, see the folllowing table) will thus make the plasma hypertonic. When the blood makes its way to the ascending limb of the loop of Henle and the PCT, the water will be returned, along the concentration gradient, to the capillaries. On the peritubular side, simply by removing the water in the descending limb, the ascending limb will have a higher concentration of ions than the plasma, thus making its movement into the capillaries possible. It may take a little effort to see it, but in the end it's worth the effort, because beneath the complexity of the details, the actual countercurrent mechanism is elegant in its simplicity!
Secretion
In addition to reabsorption of materials from the filtrate into the blood, other materials from the plasma are being placed into the filtrate in a process known as secretion (see Figure 15.6). Secretion plays a major role in the balance of ions in the blood (see the following table). Excess K+, for instance, can cause cardiac arrest, so the level can be lowered by secreting it into the collecting duct (in the presence of aldosterone).
| Reabsorption and Secretion in the Nephron | ||
|---|---|---|
| Location | Reabsorption | Secretion |
| Glomerulus (Filtration only of H2O, glucose, amino acids, Na2, Cl-, HCO3-, K+, urea, uric acid, creatinine, etc.) | None | None |
| Proximal convoluted tubule | Na+, Cl-, HCO3-, K+, H2O, glucose, urea, amino acids | H+, NH4+, creatinine |
| Descending limb, loop of Henle | H2O | urea |
| Ascending limb, loop of Henle | Na+, Cl-, K+ | urea |
| Distal convoluted tubule | Na+, Cl-, HCO3-, H2O, glucose | None |
| Collecting duct | Na+, Cl-, HCO3-, urea, H2O* | H+, K+ |

Figure 15.6Reabsorption in the DCT and ascending loop of Henle. (©Michael J. Vieira Lazaroff)
*Water is reabsorbed here as a result of ADH (anti-diuretic hormone—see Hormones).
Normal blood pH is slightly basic, falling within the narrow range of 7.35 to 7.45 (7 is neutral). When blood gets too acidic, H+ ions are secreted into the PCT and the collecting duct, thus raising the pH to normal. In addition, the blood pH can be raised by reabsorbing HCO3- (which binds with the H+ ions) from the PCT, DCT, and the collecting duct. As you can see, the use of reabsorption and secretion plays an important role in homeostasis.

Excerpted from The Complete Idiot's Guide to Anatomy and Physiology © 2004 by Michael J. Vieira Lazaroff. All rights reserved including the right of reproduction in whole or in part in any form. Used by arrangement with Alpha Books, a member of Penguin Group (USA) Inc.
To order this book direct from the publisher, visit the Penguin USA website or call 1-800-253-6476. You can also purchase this book at Amazon.com and Barnes & Noble.