Anatomy and Physiology: It's a Long Way Down
It's a Long Way Down
The mixture of masticated (chewed) food and saliva we swallow is called a bolus (sort of a big spit ball). The role of the pharynx, and especially the epiglottis, is discussed in The Respitory System. Quite an adventure will ensue, but the first leg of the journey is rather uneventful. The esophagus is less than a foot long (some 25 cm). Not being in constant use as with the trachea, it lacks the trachea's cartilaginous rings, opening mainly when we swallow. The esophagus is mainly a tube, somewhat lengthened to allow room for the thoracic organs; it doesn't even have a strong sphincter muscle at each end.
Medical Records
One of the most difficult things about the digestive system is the fact that many disorders will manifest similar systems. Heartburn or ulcers have some of the same symptoms as stomach cancer. It is often advisable to have an endoscopy when symptoms are in question. Stomach cancer, like most cancers, runs in families, so if you have a family history of it, you should be prepared to consider reducing the amount of salt in your diet. Stomach cancer is one of the few cancers to decline in the twentieth century, but for a surprising reason … the invention of refrigeration (salt was no longer needed to preserve meats)!
The muscular entrance, called the upper esophageal sphincter, is called such merely because it mimics the effect of a sphincter muscle. The exit, or the lower esophageal sphincter, is also called the cardiac sphincter, given its proximity to the heart. That name, however, sometimes causes some confusion, so it is increasingly known as the gastroesophageal sphincter. By putting the prefix gastro- before the esophagus, this helps to emphasize that the primary function of this “sphincter” is to prevent backflow, similar to, though less efficient than, the valves in the heart, in veins, and in lymphatic capillaries. When that backflow does happen, the poorly protected lining of the esophagus is digested by gastric juices, causing the sensation known as heartburn (there is no actual connection to the heart, except for the pain being felt behind the heart).
Protein Buster
Whenever people think about digestion, the first organ that comes to mind is the stomach. In fact, the stomach does very little digestion at all (liquids reside there for only about 11/2 to 21/2 hours, and solids anywhere from 3 to 4 hours). When asked to point to their stomachs, most people would probably point to the area of the umbilicus (“belly button”), and the idea of touching the bottom of the ribcage on the left side probably wouldn't occur to them. In many ways, the stomach is a surprising organ.
The Big Picture
The way to a man's heart (or a woman's for that matter) may not be through the stomach, but the way to the stomach is through the brain! The vagus nerve (N-X), a part of the parasympathetic branch of the autonomic nervous system, will increase the activity of the digestive system when the body is in a rest and repose state (as opposed to fight or flight state). If that brilliant Russian scientist, Pavlov, had been able to measure the gastric activity of his dogs, he would have found the bell triggering more than just salivation!
The expression “a full stomach” makes a lot of sense when you consider the many large folds in the lining of the gastric mucosa, known as rugae. These rugae (singular, ruga) allow the lumen of the stomach to expand after eating a large meal; you might be surprised to learn that the average adult's stomach can hold anywhere from 1 to 11/2 liters of food! Is it any wonder that some people's clothes feel tighter after a big meal?
The contents of the stomach—a mixture of food, saliva, and gastric juices—are called chyme. It may surprise you to know that your stomach gets started before you even take your first bite! This first phase of gastric activity is called the cephalic phase (cephalic = head). In this phase the gastric secretions actually start as a result of seeing, smelling, tasting, or even thinking about food!
The second phase, aptly named the gastric phase, doesn't start until the food actually enters the stomach. At this stage, the change in pH—brought about by the cephalic phase—the presence of your chewed-up meal (especially the presence of protein, the stomach's forte), and the stretching of the stomach lining by that food, get the gastric phase into full gear. Gastrin, a hormone produced by the G-cells at the very bottom of the gastric pit, will increase gastric secretion—the irony is that, as a hormone, it must make a full circuit through the blood to get to the cells that are right next door! Stretch receptors also send nervous signals that ultimately lead to greater gastric juice.
Crash Cart
It used to be believed that the best thing to do when experiencing the pain of heartburn or ulcer was to drink milk. In a way this was logical; given the acidity of the gastric juice (pH 2) and the more neutral nature of milk (pH 6.4 to 6.8), the combination of the two does, if not produce a neutralization reaction, at least dilute the stomach acid and thus raise the pH. Any relief, however, is temporary, because ultimately the protein in the milk will increase the gastric secretions, making the pain even worse!
The last phase, which starts up to four hours after the start of the gastric phase, is quite sensibly named the intestinal phase, is the one in which, as you can imagine, the chyme is sent on its merry way into the first part of the small intestine, the duodenum, through the pyloric sphincter (in this case, a real sphincter). The lion's share of the digestion happens in the small intestine, so it is important that the digestion happens efficiently. If too much food enters the small intestine at once, the enzymes will not be able to digest it all effectively.
This is regulated by something called the enterogastric reflex, in which a slowing of gastric contractions follows the “squirting” of chyme into the duodenum. This prevents too much chyme from entering the duodenum at once, and also enables the duodenum to prepare, through the production of extra buffers, to counteract the low pH of the gastric chyme. If this regulation doesn't function properly, a duodenal ulcer is the result!
Flex Your Muscles
In remembering the three gastric phases, concentrate on the other areas of the body involved. The cephalic phase is triggered by nerve impulses from the brain when you think about food. The gastric phase concentrates on the actions of the stomach itself once the food actually enters the stomach. Lastly, the intestinal phase is, quite simply, the phase where the contents of the stomach actually enter the duodenum of the small intestine through the pyloric sphincter.
Okay, you get the idea that the stomach releases digestive enzymes to digest proteins, but aren't there proteins on the outside of every cell, including those that line the stomach? So how does the stomach keep from digesting itself after pumping out so much stomach acid and enzymes? For one thing, it doesn't always! Sometimes the stomach starts to digest its own lining, basically turning itself into a cannibal! That, in a nutshell, is the basis of an ulcer—I know some people get hungry from time to time, but really! Still, most people never develop ulcers, so how does the stomach keep from eating itself?
Medical Records
To understand the three types of ulcers, refer to the layers of the typical digestive organ. Since extracellular digestion occurs in the lumen of the stomach, either a lack of mucus or an excess of HCl can cause extracellular digestion—digestion of the mucosa itself. The simplest ulcer is just this, and is a reddening of the gastric mucosa. Since the epithelium of the mucosa is avascular, there would be no bleeding. A bleeding ulcer involves digestion of the submucosa's vascular connective tissue (gastric juice makes blood turn black). If the bleeding isn't enough to stop you, and the digestion continues through the muscularis and the serosa, the perforation of the stomach wall gives this type of ulcer its name: a perforated ulcer.
For one thing, the gastric mucosa (which lines the lumen) makes good on its name and churns out large quantities of mucus. Since mucus is made of water, protein, and polysaccharides, the water helps to dilute the acid, thus raising (buffering) the pH of the gastric juice closest to the mucosa; the enzyme pepsin gets to work on the mucous proteins, rather than the mucosal proteins! That is all well and good, but what about when the HCl and the pepsin are first released? What protects the cells then?
Medical Records
HCl acid does more than activate the pepsin. Proteins are so complex that their digestion is a long process. The HCl acid breaks the hydrogen bonds that make the secondary, tertiary, and quaternary structures of the proteins, making it easier to break the peptide bonds in the primary structure. The HCl acid also breaks down plant cell walls (although we cannot actually digest the cellulose in them), not to mention breaking down the connective tissue in meat. The HCl acid also helps to kill bacteria in food. This, however, is not foolproof, because certain bacteria can make it past the stomach's defenses, not to mention the recent discovery of Helicobacter pylori, the species of bacteria whose daily activity is the cause of many gastric ulcers!
In a tricky maneuver, the stomach takes advantage of the shape of the gastric mucosa, and a little chemical trickery, to get away with it (see Figure 14.3)! The gastric mucosa is filled with pits called gastric pits. At the base of these pits are chief cells, which release pepsinogen, an inactive form of the enzyme pepsin. Being inactive, the protein poses no problem for the mucosa. At the neck of these gastric pits are parietal cells, which release HCl acid. That alone would be a problem, but for the cell's clever habit of releasing H+ ions and Cl ions separately, thus protecting itself from the HCl acid! Sure, fine, but how does the pepsinogen turn into pepsin? By mixing with the HCl acid! Those two don't mix until they meet in the neck of the gastric pit, and the enzyme doesn't become active right away, thus buying enough time to wait for the chemicals to reach the lumen! This is just one more example of how true understanding of the anatomy of the body (in this case, of the gastric pits) is only understood when one also looks at the physiology!
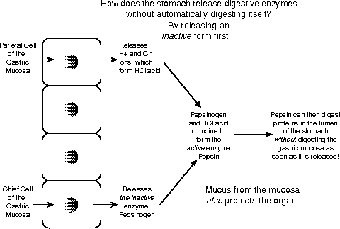
Figure 14.3Why enzymes are released in an inactive form. (©Michael J. Vieira Lazaroff)
The greatest risk when the stomach starts digesting itself is that such an ulcer can actually digest so deep a hole in the stomach wall that an opening is made into the abdominal cavity; this is called a perforated ulcer. Luckily, the body has an ace up its sleeve in a somewhat disgusting sheet of connective tissue called the greater omentum (see Figure 14.4). This sheet literally hangs down in front of the small intestine, acting in part as a place for depositing excess fat, but more importantly, the greater omentum can adhere to any perforations in the stomach wall, thus preventing the contents from emptying into the abdominal cavity. There is also a lesser omentum, but it just connects the liver to the stomach.

Figure 14.4This sagittal section shows the organs within the lesser omentum and the greater omentum, as well as the intestinal mesentery. www.clipart.com

Excerpted from The Complete Idiot's Guide to Anatomy and Physiology © 2004 by Michael J. Vieira Lazaroff. All rights reserved including the right of reproduction in whole or in part in any form. Used by arrangement with Alpha Books, a member of Penguin Group (USA) Inc.
To order this book direct from the publisher, visit the Penguin USA website or call 1-800-253-6476. You can also purchase this book at Amazon.com and Barnes & Noble.
